Diabetes NCLEX Practice Questions For Nursing Proficiency In 2023
As a nursing professional, you understand the critical role you play in empowering individuals living with diabetes to lead fulfilling lives while managing their condition effectively. The National Council Licensure Examination (NCLEX) evaluates your competency to provide safe and competent care, making it essential to be thoroughly prepared for any diabetes-related scenarios you may encounter during the exam.
In this blog, we have crafted a set of diabetes NCLEX questions from Smart’n. This set of NCLEX practice questions helps you build the confidence and knowledge necessary to ace your NCLEX and, more importantly, to excel in your nursing career.
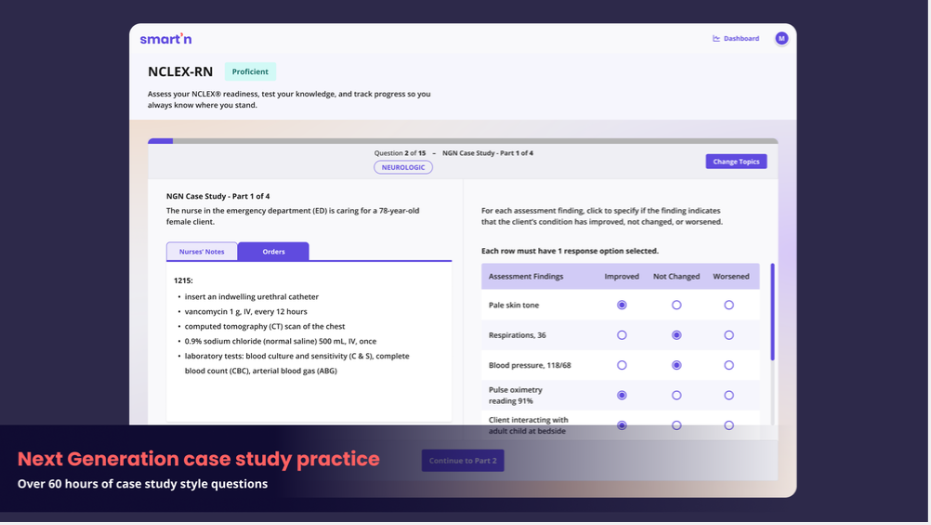
Smart'n is an NCLEX study tool specifically created to aid nursing students in their studies. It offers a comprehensive collection of resources, including practice questions, detailed explanations (rationales), and assessments.
With access to over 2,500 practice questions and 60+ hours of NGN NCLEX-style nursing case studies, students can access concise NextGen content organized by topic.
This enables them to focus on specific areas of nursing practice, such as respiratory, cardiac, mental health, neurological, and others, making their learning process more effective and targeted.
Understanding the NCLEX questions on diabetes
Understanding NCLEX diabetes nursing questions requires familiarity with the key concepts related to this condition and the approach to answering NCLEX-style questions. Here are some important points to keep in mind:
Know the basics
Understand the pathophysiology of diabetes mellitus, including the types (Type 1, Type 2, gestational diabetes), risk factors, signs and symptoms, complications (e.g., hyperglycemia, hypoglycemia, ketoacidosis), and management strategies (e.g., insulin therapy, oral antidiabetic medications, lifestyle modifications).
Assess and prioritize
When presented with a diabetes-related question, carefully assess the patient's condition and prioritize interventions based on the ABCs (Airway, Breathing, Circulation). Address any immediate life-threatening issues first.
Consider comorbidities
Diabetes often coexists with other conditions, such as hypertension, cardiovascular disease, and renal impairment. Be aware of potential complications and interactions with other medications.
Lifestyle modifications
Understand the significance of diet, exercise, and blood glucose monitoring in diabetes management. These are key components of patient education.
Medication management
Familiarize yourself with common antidiabetic medications, their mechanisms of action, side effects, and indications for use.
Sick day management
Know the specific measures for managing diabetes during illness, as it can impact blood glucose levels.
Long-term complications
Be aware of the potential long-term complications of diabetes, such as neuropathy, nephropathy, and retinopathy.
Patient education
Consider the patient's understanding of their condition and their ability to manage it. Patient education is essential in diabetes management.
Safety measures
Consider patient safety in the context of diabetes management. For example, avoiding foot injuries, preventing infection, and monitoring for hypoglycemia.
Diabetes NCLEX questions
Let’s check some of Smart’n’s Diabetes NCLEX practice questions with their answers and rationals:
Question One
A nurse is caring for a client with an exacerbation of chronic obstructive pulmonary disease (COPD) and a history of type 2 diabetes mellitus requiring insulin. The client has been prescribed prednisone. The nurse anticipates which need?
Close monitoring for hypotension
Gradually increasing the prednisone dose
Increasing the insulin dose
Monitoring and recording intake and output
A. Incorrect Answer
Close monitoring for hypotension
Rationale: Most glucocorticoids have some mineralocorticoid activity, causing fluid retention and worsening hypertension.
B. Incorrect Answer
Gradually increasing the prednisone dose
Rationale: Prednisone is started at a higher dose and then gradually decreased for COPD exacerbation and most other conditions. A slow taper will prevent adrenal crisis.
C. Correct Answer
Increasing the insulin dose
Rationale: Corticosteroids (e.g., methylprednisolone, prednisone, dexamethasone) are given to combat inflammation in the lungs in clients with COPD exacerbation. All glucocorticoids can cause an increase in blood sugar. This may lead to the need for a higher dose of insulin based on the client's blood sugar level.
D. Incorrect Answer
Monitoring and recording intake and output
Rationale: Intake and output are not affected by corticosteroids.
Question Two
The nurse is caring for a diabetic client who takes insulin. Which of the following actions should the nurse take to avoid complications?
Encourage discarding the needles in the garbage
Reuse syringes for a week before replacing
Rotate sites for providing insulin
Mix long acting insulin first
A. Incorrect Answer
Encourage discarding the needles in the garbage
Rationale: A plastic biohazard container is best, although a client may not have access to this. If not, a thick plastic container with a lid is acceptable.
B. Incorrect Answer
Reuse syringes for a week before replacing
Rationale: Needles should be used once and then discarded.
C. Correct Answer
Rotate sites for providing insulin
Rationale: The nurse should rotate sites for providing insulin to avoid lipodystrophy, which affects insulin absorption and distribution.
D. Incorrect Answer
Mix long acting insulin first
Rationale: Regular insulin is drawn up first.
Question Three
A nurse is caring for a client who has developed diabetic ketoacidosis. The client has a breathing pattern in which he takes rapid and very deep breaths with large tidal volumes. Which of the following best describes this type of breathing?
Biot's respiration
Paroxysmal nocturnal dyspnea
Kussmaul's respirations
Cheyne-Stokes respirations
A. Incorrect Answer
Biot's respiration
Rationale: This refers to quick, shallow respirations followed by periods of apnea, indicating a neurological problem.
B. Incorrect Answer
Paroxysmal nocturnal dyspnea
Rationale: This breathing pattern is characterized by periods of severe dyspnea during sleep that wakens the client. This is common in the client with heart failure.
C. Correct Answer
Kussmaul's respirations
Rationale: Kussmaul's respirations involve an abnormal pattern of breathing that is often associated with a condition of metabolic acidosis, such as with diabetic ketoacidosis. Kussmaul's respirations are characterized by a rapid breathing rate in which the client takes very deep breaths. The client may breathe in this manner when the body is trying to compensate for metabolic acidosis.
D. Incorrect Answer
Cheyne-Stokes respirations
Rationale: Cheyne-Stokes respirations are characterized by rhythmic breathing with periods of apnea. This breathing pattern can indicate a brain problem or metabolic dysfunction.
Question Four
A home care nurse is working with a diabetic client with poor tissue perfusion. Based on the nurse’s knowledge of this condition, which of the following effects would the nurse most likely see in the client’s extremities?
Increased venous return
3+ peripheral pulses
Poor hair and nail growth
Sweaty skin
A. Incorrect Answer
Increased venous return
Rationale: This is a manifestation of increased blood flow. In contrast, the client with poor tissue perfusion would have decreased venous return, not the other way around.
B. Incorrect Answer
3+ peripheral pulses
Rationale: This is a manifestation of increased blood flow. In contrast, the client with poor tissue perfusion would have weaker pulses, decreased venous return, and cool, clammy skin.
C. Correct Answer
Poor hair and nail growth
Rationale: A client with poor tissue perfusion will likely demonstrate abnormal patterns of hair and nail growth on the hands and feet. This occurs because of peripheral arterial disease (PAD). PAD is a chronic disorder in which the lower extremities are deprived of nutrients and oxygen due to impaired arterial blood flow, resulting in tissue damage, pain, hair loss, dry skin, thickened toenails, and cold skin in the lower extremities.
D. Incorrect Answer
Sweaty skin
Rationale: This is also a manifestation of increased blood flow. The client with poor tissue perfusion would have cool, clammy skin.
Question Five
A nurse is educating a newly diagnosed diabetic client about what to do when they are sick. Which of the following statements by the client demonstrates that further education is necessary?
"I can go ahead and double my insulin dosages while sick."
"My blood sugars may be elevated if I am sick."
"I'll make sure to test my urine for ketones."
"It's important to try to keep fluids down even if I am feeling ill."
A. Correct Answer
"I can go ahead and double my insulin dosages while sick."
Rationale: When sick, a client with diabetes may experience higher blood sugars, but insulin dosages should continue to be based on the actual blood sugar level and food intake. Clients should not simply double their insulin levels, this would not be appropriate.
B. Incorrect Answer
"My blood sugars may be elevated if I am sick."
Rationale: Due to extra stress on the body, diabetic clients may experience elevated blood sugars when they are sick. It's important to continue to monitor their blood sugars closely during periods of illness.
C. Incorrect Answer
"I'll make sure to test my urine for ketones."
Rationale: It is possible for a client who is ill to develop diabetic ketoacidosis or see higher levels of ketones in their urine. It is important for clients to test their urine for ketones at least daily, or more often if instructed.
D. Incorrect Answer
"It's important to try to keep fluids down even if I am feeling ill."
Rationale: Clients should be instructed to ensure adequate or increased fluid intake to prevent dehydration.
If you are looking for more diabetes nursing questions, you can use Smart’n. It provides you with NCLEX practice question banks.
Conclusion
In conclusion, mastering Diabetes NCLEX practice questions is an indispensable skill for nursing proficiency in 2023 and beyond. As the healthcare landscape continues to evolve, the prevalence of diabetes remains a significant challenge, placing nurses on the frontlines of patient care. NCLEX practice questions focused on diabetes offer valuable opportunities to enhance our knowledge, critical thinking, and problem-solving abilities, ensuring that we are well-equipped to provide optimal care to individuals living with this chronic condition.
FAQs
1- Do the first 15 questions count on NCLEX?
The initial fifteen questions serve as pretest items and do not contribute to the exam's scoring or the assessment of a test-taker's passing status in the NCLEX-RN.
2- What score do I need to pass NCLEX?
The NCLEX employs a baseline logit score of 0.00 as a threshold to determine the pass or fail outcome. To pass, a candidate must achieve a score above 0.00, indicating that they have answered a sufficient number of questions correctly. Conversely, a negative score indicates that the candidate did not answer enough questions correctly to meet the passing criteria.