5 Nursing Case Study Examples + Answer Guide
If you're a nursing student preparing for your nursing license exam, you know how important it is to have access to high-quality study materials.
Sample case study for nursing students can be a valuable tool in your preparation, helping you to develop critical thinking skills and apply your knowledge in real-world scenarios.
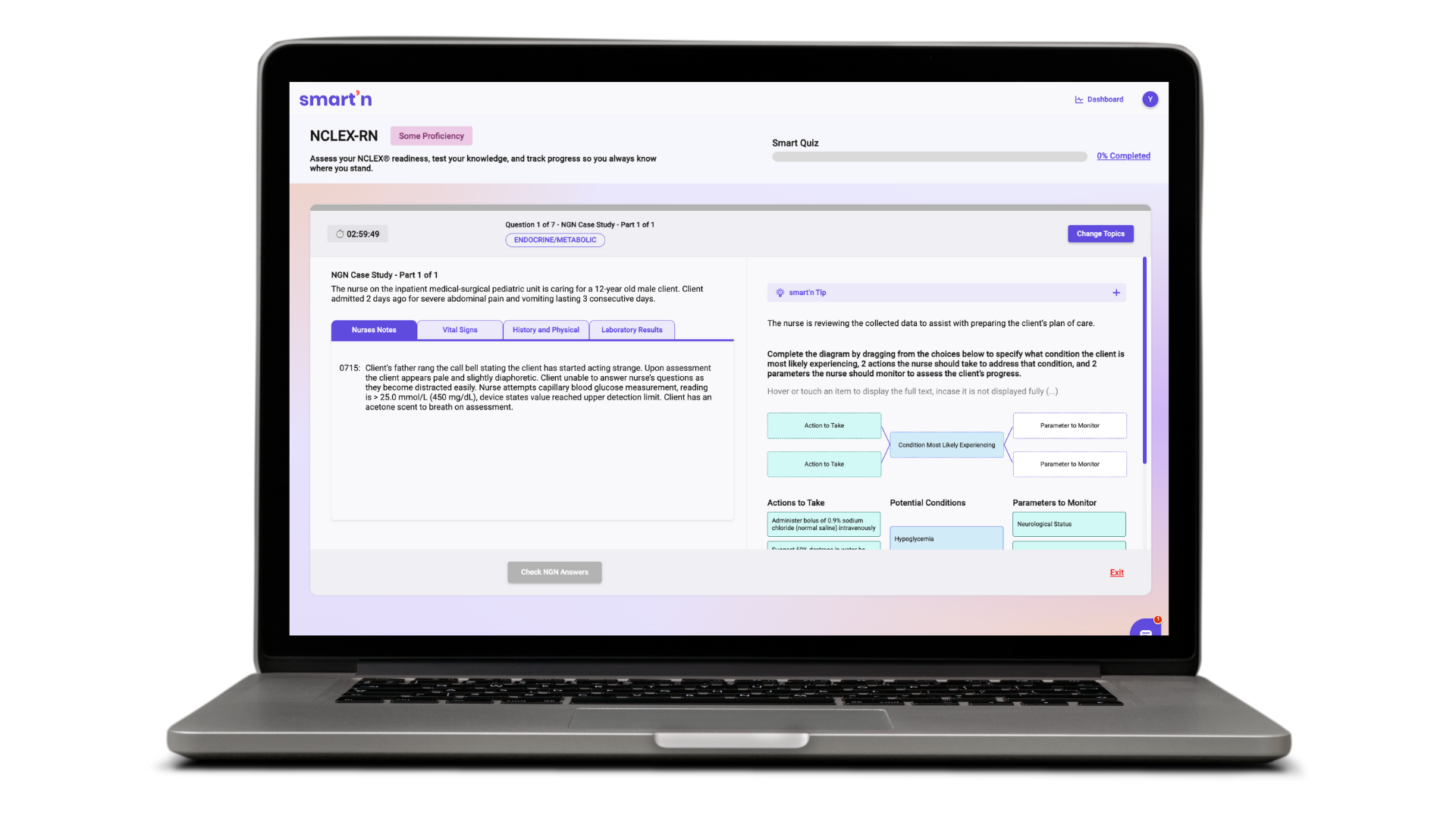
That's why we've put together a list of 5 nursing case study examples, complete with answer guides, to help you prepare for the NCLEX-style questions you'll encounter on exam day. You can also generate a case study question like the one you will see on the exam; just ask Smart’n.
Nursing Case Study: Mrs. Johnson's hypertension
Background of Mrs. Johnson’s hypertension
Mrs. Johnson is a 62-year-old female who was admitted to the hospital with a complaint of severe headache and dizziness. She has a past medical history of hypertension for the past 5 years, and she has been on antihypertensive medications.
She has a family history of hypertension and heart disease, with her mother and brother both diagnosed with hypertension. Mrs. Johnson is currently working as a school teacher and lives with her husband. She has a sedentary lifestyle and reports occasional non-adherence to her medications due to forgetfulness.
Nurse notes of Mrs. Johnson’s hypertension
Upon admission, Mrs. Johnson's vital signs are as follows: blood pressure (BP) 180/100 mmHg, heart rate (HR) 88 beats per minute (BPM), respiratory rate (RR) 18 breaths per minute, and temperature 98.6°F.
She is alert and oriented but complains of a throbbing headache and lightheadedness. Her skin is warm and dry, and there is no visible edema. Her lungs are clear on auscultation, and her heart sounds are normal with no murmurs. Her abdominal assessment reveals no tenderness or masses. Mrs. Johnson's laboratory results show an elevated fasting blood glucose level of 135 mg/dL, cholesterol level of 240 mg/dL, and serum creatinine level of 1.2 mg/dL. She has a body mass index (BMI) of 30, which indicates obesity.
Questions and answer guide of case study
1. What are the risk factors for hypertension in this case study?
Family history of hypertension and heart disease
Sedentary lifestyle
Non-adherence to medications
2. What are the signs and symptoms of hypertension in Mrs. Johnson?
Severe headache
Dizziness
Elevated blood pressure (180/100 mmHg)
3. What other assessments should the nurse prioritize for Mrs. Johnson?
Regular monitoring of blood pressure
Monitoring of blood glucose and cholesterol levels
Assessment of adherence to medications
Assessment of lifestyle factors, such as physical activity and diet
4. What nursing interventions would be appropriate for Mrs. Johnson's hypertension management?
Administer antihypertensive medications as ordered
Educate Mrs. Johnson and her husband on the importance of medication adherence
Encourage regular physical activity and a healthy diet
Monitor and manage blood glucose and cholesterol levels
Provide education on stress management techniques
Collaborate with the healthcare provider to adjust medications and treatment plans as needed
5. What patient education should the nurse provide to Mrs. Johnson regarding hypertension management?
Importance of adhering to antihypertensive medications as prescribed
Adoption of a healthy lifestyle, including regular exercise and a well-balanced diet
Monitoring and management of blood glucose and cholesterol levels
Strategies for stress management
Importance of regular follow-up appointments with the healthcare provider for monitoring and adjustments to the treatment plan
6. What referrals or consultations should the nurse consider for Mrs. Johnson?
Registered dietitian for nutritional counselling
A social worker for assistance with lifestyle modifications and stress management
Diabetes educator for management of blood glucose levels
Pharmacist for medication review and education
Healthcare provider for possible adjustment of antihypertensive medications or referral to a specialist, such as a cardiologist or endocrinologist.
Want access to 25 more unfolding case studies with answer rationales?
Sign up to Smart’n to access, for a limited time it’s free for students and aspiring nurses.
Nursing Case Study: Mr. Thompson's diabetic foot ulcer
Background of Mr. Thompson’s diabetic foot ulcer
Mr. Thompson is a 68-year-old male with a history of type 2 diabetes for the past 15 years. He has a sedentary lifestyle and a BMI of 32, indicating obesity. Mr. Thompson has a history of poor glycemic control with frequent episodes of hyperglycemia and occasional non-adherence to his diabetic medications due to financial constraints.
He presents to the clinic with a complaint of a non-healing ulcer on his right foot for the past 2 weeks. He reports that he accidentally bumped his foot against a hard object and developed a small blister that has since progressed to a deep, painful ulcer with foul-smelling drainage.
Assessment of Mr. Thompson’s diabetic foot ulcer
Upon assessment, Mr. Thompson's vital signs are stable with a blood pressure (BP) of 132/82 mmHg, heart rate (HR) of 76 beats per minute (BPM), respiratory rate (RR) of 18 breaths per minute, and temperature of 98.2°F.
He appears anxious and in mild distress due to the pain from the foot ulcer. His right foot is swollen, erythematous, and warm to the touch, with a deep, irregularly-shaped ulcer measuring approximately 3 cm x 4 cm on the plantar surface.
There is purulent drainage with a foul odor, and the surrounding skin is macerated. Mr. Thompson has diminished sensation in his right foot and a weak dorsalis pedis pulse. His laboratory results show an elevated fasting blood glucose level of 240 mg/dL and a hemoglobin A1c level of 9.5%.
Questions and answer guide of case study
1. What are the risk factors for the development of diabetic foot ulcer in Mr. Thompson?
History of type 2 diabetes for 15 years
Poor glycemic control with frequent episodes of hyperglycemia
Non-adherence to diabetic medications
Sedentary lifestyle and obesity
Foot injury due to accidental trauma
2. What are the signs and symptoms of the diabetic foot ulcer in Mr. Thompson?
Deep, irregularly-shaped ulcer with foul-smelling drainage
Swollen, erythematous, and warm foot
Macerated skin surrounding the ulcer
Diminished sensation and weak pulse in the affected foot
3. What other assessments should the nurse prioritize for Mr. Thompson's diabetic foot ulcer management?
Assessment of pain level and pain management
Assessment of wound characteristics, including size, depth, drainage, odor, and surrounding skin condition
Neurovascular assessment, including sensation, pulses, and skin temperature
Assessment of glycemic control and diabetes management
Assessment of nutritional status and hydration
4. What nursing interventions would be appropriate for Mr. Thompson's diabetic foot ulcer management?
Administering prescribed analgesics for pain management
Performing wound care, including cleansing, debridement, and dressing changes
Educating Mr. Thompson on proper foot care, including daily inspection, keeping the foot clean and dry, and avoiding trauma
Assisting with glycemic control through medication administration, dietary management, and regular blood glucose monitoring
Facilitating referrals to a wound care specialist, podiatrist, or diabetes educator as needed
Educating Mr. Thompson and his family on the importance of adherence to diabetic medications and lifestyle modifications
5. What patient education should the nurse provide to Mr. Thompson regarding diabetic foot ulcer management?
Proper foot care techniques, including daily foot inspection, keeping the foot clean and dry, and avoiding trauma
Importance of adherence to diabetic medications and lifestyle modifications for glycemic control
Signs and symptoms of infection, such as increased pain, redness, swelling, or drainage, and when to seek medical attention
Appropriate footwear selection and fitting to prevent further foot injury
Importance of regular follow-up appointments with healthcare providers for ongoing monitoring and management of diabetes and foot ulcer
Nutritional recommendations for diabetes management, including a balanced diet and avoiding high-sugar foods and beverages
Importance of maintaining a healthy weight through lifestyle modifications, including regular physical activity and healthy eating habits
Emphasizing the need for strict glycemic control to promote wound healing and prevent complications
Instruction on the proper administration of prescribed medications, including dosages, timing, and potential side effects
Education on the risks and consequences of non-adherence to diabetes management and foot care recommendations
6. What interdisciplinary team members may be involved in Mr. Thompson's diabetic foot ulcer management?
Primary care physician or endocrinologist for diabetes management
Wound care specialist or podiatrist for specialized wound care and management
Diabetes educator for diabetes education and self-management strategies
Registered dietitian for nutritional counseling
Pharmacist for medication management and education
Physical therapist for recommendations on appropriate physical activity and exercise
A social worker or financial counselor for assistance with financial constraints related to medication affordability
Ask Smart’n, the GPT for nurses to build you a case study like one you wlll see on the NCLEX exam
Nursing Case Study: Mich’s chest pain
Background of Mich’s chest pain
Mich is a 15-year-old male who was brought to the emergency department by his parents due to complaints of chest pain and shortness of breath. Mich has a history of asthma and had been experiencing symptoms for the past two days. Mich's parents reported that he had been compliant with his asthma medications but had recently run out of his inhaler. Upon arrival at the emergency department, Mich was found to have a rapid heart rate and was diagnosed with a severe asthma exacerbation.
Assessment of Mich’s chest pain
On assessment, Mich appeared anxious and in distress, with labored breathing and a respiratory rate of 30 breaths per minute. His oxygen saturation was 88% on room air, and he was immediately started on supplemental oxygen via nasal cannula.
Mich's chest exam was significant for decreased breath sounds and wheezing. His heart rate was 130 beats per minute, and his blood pressure was 120/70 mmHg. Mich's laboratory values were within normal limits, except for an elevated white blood cell count, which was likely due to his asthma exacerbation.
Questions and answer guide of case study
1. What is the priority nursing intervention for Mich?
The priority nursing intervention for Mich is to assess and manage his respiratory distress. This includes providing supplemental oxygen, administering bronchodilator medications, and monitoring his response to treatment.
2. What education should the nurse provide to Mich and his parents?
The nurse should educate Mich and his parents on the proper use of asthma medications, including inhalers and nebulizers. The nurse should also provide education on asthma triggers and how to avoid them, as well as signs and symptoms of an asthma exacerbation and when to seek medical attention.
3. What potential complications should the nurse monitor for in Mich?
The nurse should monitor Mich for potential complications of asthma exacerbation, including respiratory failure, pneumothorax, and cardiac complications such as arrhythmias. The nurse should also monitor for signs of anxiety and provide emotional support to Mich and his family.
4. How can the nurse promote adherence to Mich's asthma treatment regimen?
The nurse can promote adherence to Mich's asthma treatment regimen by providing education and resources, such as written instructions and referrals to support groups. The nurse can also encourage open communication with Mich and his family and address any barriers to adherence, such as cost or access to medications.
5. What discharge planning should the nurse initiate for Mich?
The nurse should initiate discharge planning that includes instructions for Mich and his family on proper asthma management at home. This includes providing education on medication administration, recognizing signs and symptoms of asthma exacerbation, and developing an asthma action plan. The nurse should also ensure that Mich has access to his medications and any necessary equipment, such as a peak flow meter or spacer. Referral to a primary care provider or asthma specialist for ongoing management should also be initiated. Finally, the nurse should provide education on follow-up appointments and any necessary referrals for additional support services, such as social work or mental health resources.
6. How can the nurse promote family-centered care for Mich and his parents?
The nurse can promote family-centered care by involving Mich and his parents in the care planning process and encouraging their participation in decision-making. The nurse can provide emotional support and education to help them feel confident in their role as caregivers, and address any cultural or religious needs of the family to promote a holistic approach to care. The nurse should also encourage family visitation and provide opportunities for Mich and his parents to ask questions and express concerns.
Nursing Case Study: Baby S - Respiratory distress and hypoxemia
Background of baby’s respiratory distress and hypoxemia
Baby S is a 10-day-old infant who was admitted to the neonatal intensive care unit (NICU) due to respiratory distress and hypoxemia. Baby S was born prematurely at 34 weeks gestation via emergency cesarean section due to fetal distress.
The mother had a history of preeclampsia and received antenatal corticosteroids. Baby S had a birth weight of 2.2 kg and required immediate intubation and mechanical ventilation.
Assessment of baby’s respiratory distress and hypoxemia
On assessment, Baby S appeared to be in moderate respiratory distress, with a respiratory rate of 50 breaths per minute, nasal flaring, and intercostal retractions. Her oxygen saturation was 88% on a fraction of inspired oxygen (FiO2) of 0.5, and her heart rate was 160 beats per minute. Lung auscultation revealed bilateral crackles, and the chest X-ray showed diffuse bilateral infiltrates consistent with respiratory distress syndrome (RDS). Baby S had a central line for parenteral nutrition and was receiving intravenous fluids and medications.
Questions and answer guide of case study
1. What is the pathophysiology of RDS in premature infants?
RDS is a common respiratory disorder in premature infants, caused by a deficiency of pulmonary surfactant, which normally keeps the alveoli open and prevents collapse. In premature infants, the lungs are not fully developed, and surfactant production is inadequate, leading to increased surface tension and collapse of the alveoli. This results in ventilation-perfusion (V/Q) mismatch, hypoxemia, and respiratory distress.
2. What interventions should the nurse implement for Baby S?
The nurse should ensure that Baby S is receiving appropriate respiratory support, including mechanical ventilation, FiO2 titration, and positive end-expiratory pressure (PEEP) as prescribed. The nurse should also monitor Baby S's vital signs, oxygen saturation, and blood gas values closely to optimize oxygenation and ventilation. The nurse should maintain a sterile environment around the central line and monitor for signs of infection. The nurse should also provide enteral or parenteral nutrition as prescribed to meet the infant's metabolic needs and promote growth.
3. What potential complications should the nurse monitor for in Baby S?
The nurse should monitor for potential complications such as infection, barotrauma, bronchopulmonary dysplasia (BPD), and patent ductus arteriosus (PDA). Infection is a common complication in premature infants and can be life-threatening. Barotrauma can occur due to excessive mechanical ventilation and can result in pneumothorax or other complications. BPD is a chronic lung disease that can develop in premature infants who require prolonged mechanical ventilation or oxygen therapy. PDA is a common cardiac complication in premature infants, resulting in abnormal blood flow between the aorta and pulmonary artery.
4. How can the nurse support Baby S's developmental care needs?
The nurse can support Baby S's developmental care needs by providing a quiet and dark environment, minimizing unnecessary handling and stimulation, and promoting restful sleep. The nurse can also encourage skin-to-skin contact with the mother or father to promote bonding and provide comfort. The nurse should also provide appropriate pain management for any procedures or interventions to minimize discomfort and stress.
5. What discharge planning should the nurse initiate for Baby S?
The nurse should initiate discharge planning as early as possible to ensure a smooth transition to home. The nurse should provide education to the parents about the infant's medical needs, including respiratory support, feeding, medication administration, and infection prevention. The nurse should also refer the parents to appropriate community resources, such as home health services, support groups, and developmental follow-up clinics. The nurse should work with the healthcare team to develop a plan for ongoing monitoring and follow-up to ensure that Baby S's medical needs are being met and to monitor for any potential complications or developmental delays.
6. How can the nurse promote family-centered care for Baby S and her parents?
The nurse can do so by involving the parents in the infant's care as much as possible, encouraging their participation in decision-making, and providing emotional support and education to help them feel confident in their role as caregivers. The nurse can also encourage family visitation and provide opportunities for parent-infant bonding, such as skin-to-skin contact and feeding. The nurse should also recognize and address any cultural or religious needs of the family to promote a holistic approach to care.
Nursing Case Study: Mrs. Jones - Postoperative care after total hip replacement surgery
Background of Mrs. Jones’ hip replacement surgery
Mrs. Jones is a 72-year-old female who underwent total hip replacement surgery due to severe hip osteoarthritis. She has a history of hypertension and osteoporosis. Mrs. Jones lives alone and has limited mobility due to hip pain and stiffness prior to surgery. She was admitted to the orthopedic surgical unit and is now postoperative day 1 after her surgery.
Assessment of Mrs. Jones’ hip replacement surgery
Mrs. Jones is alert and oriented but reports pain at the surgical site rated 7/10 on the pain scale.
Vital signs: Blood pressure 140/90 mmHg, heart rate 88 bpm, respiratory rate 18 bpm, temperature 98.6°F.
Surgical incision: 15 cm incision over the lateral aspect of the right hip, with moderate serosanguinous drainage.
Limited weight-bearing status on the right leg as per surgeon's orders.
Foley catheter in place for urinary drainage.
Serosanguinous drainage in the surgical drain.
Evaluation of Mrs. Jones’ hip replacement surgery
Mrs. Jones's pain is well managed, with her pain level reduced to 4/10 on the pain scale within 24 hours post-surgery.
Mrs. Jones is able to perform transfers and ambulation with appropriate assistive devices as per the prescribed weight-bearing status.
There are no signs of infection at the surgical site or systemic infection.
Mrs. Jones and her family demonstrate an understanding of the postoperative care plan, including pain management, mobility restrictions, and infection prevention measures.
Mrs. Jones's home environment is assessed to be safe for her discharge, and necessary home health services, medical equipment, or rehabilitation services are arranged.
Questions and answer guide of Case Study
1. What are the priority nursing diagnoses for Mrs. Jones?
Acute Pain related to surgical incision and tissue trauma
Impaired Physical Mobility related to postoperative weight-bearing restrictions
Risk for Infection related to the surgical site and indwelling catheter
2. What are the nursing interventions to address Mrs. Jones's acute pain?
Assess pain level using a numeric pain scale at regular intervals and as needed.
Administer prescribed pain medications, such as acetaminophen and opioids, as ordered and monitor for side effects.
Apply ice or heat to the surgical site as appropriate to help relieve pain and reduce swelling.
Use non-pharmacological pain relief measures, such as relaxation techniques and distraction techniques, to help Mrs. Jones manage her pain.
3. How can the nursing team assist Mrs. Jones with impaired physical mobility?
Assist Mrs. Jones with transferring and ambulation according to the prescribed weight-bearing status and mobility orders.
Educate Mrs. Jones on the proper use of assistive devices, such as crutches or a walker, and provide assistance as needed.
Collaborate with the physical therapy team to develop a plan of care for Mrs. Jones's mobility and ambulation post-surgery.
Encourage Mrs. Jones to perform a range of motion exercises as tolerated to prevent joint stiffness and muscle atrophy.
4. What nursing interventions can be implemented to prevent infection in Mrs. Jones?
Perform frequent hand hygiene and use appropriate personal protective equipment (PPE) when providing care to Mrs. Jones, especially when handling the surgical drain or catheter.
Monitor the surgical incision for signs of infection, such as redness, increased warmth, swelling, or purulent drainage, and report any abnormal findings to the healthcare provider.
Monitor vital signs, including temperature, for signs of systemic infection.
Ensure proper care and maintenance of the indwelling catheter according to the facility's policy and procedure.
5. What should be included in Mrs. Jones's education and discharge planning?
Provide Mrs. Jones and her family with education on the postoperative care plan, including pain management, mobility restrictions, and infection prevention measures.
Provide written materials and verbal instructions on wound care, medication administration, activity restrictions, and follow-up appointments.
Collaborate with the interdisciplinary team, including the physical therapist and social worker, to assess Mrs. Jones's home environment and ensure a safe discharge plan.
Assist with coordinating any necessary home health services, medical equipment, or rehabilitation services for Mrs. Jones's post-discharge care.
6. How will the nursing team evaluate the effectiveness of the care provided to Mrs. Jones?
Monitor Mrs. Jones's pain level and assess for any side effects of pain medications.
Assess Mrs. Jones's ability to perform transfers and ambulation with assistive devices.
Monitor the surgical incision and vital signs for signs of infection.
Evaluate Mrs. Jones's and her family's understanding of the education provided and their ability to implement the postoperative care plan.
Collaborate with the interdisciplinary team to ensure a safe and appropriate discharge plan for Mrs. Jones.
Want to access 25 more case studies with full-answer rationales?
Nurses can ask Smart’n anything for instant, trustworty answers—and access 25 top NCLEX case-studies in study mode.